Archive
Administration keeping records hidden and declining comment on COVID-19 in DDS system
The Baker administration seems to be going out of its way to avoid providing information to us regarding the impact COVID-19 has had on persons with intellectual and developmental disabilities in Massachusetts.
We have four outstanding Public Records Requests with three state agencies – the Executive Office of Health and Human Services (EOHHS), the Department of Developmental Services (DDS), and the Department of Public Health (DPH). In none of the cases have we received responsive documents.
Administration officials also don’t appear even to want to talk about their response to the pandemic. Neither HHS Secretary Marylou Sudders nor DDS Commissioner Jane Ryder have responded to our repeated questions over the past several months about the lack of mandatory testing of staff in the DDS system for COVID-19.
A key state lawmaker also declined to clarify her apparently erroneous remarks recently made to a COFAR member about why mandatory testing of staff isn’t being done. (More about that below.)
Ryder also has refused to respond to our questions about the administration’s apparently haphazard policy on retesting of persons in the system or the slow pace of testing of both residents and staff.
For instance, one parent of a resident in a state-operated group home said his daughter has been tested four times in her group home since April, and has been negative each time. Meanwhile, approximately 1,400 residents in the DDS system haven’t even been tested once.
We are concerned that if a second wave of the virus hits Massachusetts, DDS’s lack of a coherent policy on retesting could be tragic.
No mandatory testing records provided
Our longest-running Public Records request to the administration is for internal emails and other documents relating to the topic of mandatory testing of staff in the DDS system. As we have reported, DDS does not require staff to be tested even though it is likely that much of the spread of the virus in group homes has been caused by asymptomatic staff.
I first asked EOHHS, DDS, and DPH on May 26, more than a month and a half ago, for emails and other records regarding mandatory testing, and so far none have been provided. The stories keep changing from EOHHS as to whether they have any such records.
First, EOHHS said in early June that they had so many records that the cost could potentially be prohibitive to provide them to us. But after I narrowed down my request at their suggestion, they said earlier this month that they have no responsive records. I filed an appeal with the state Public Records Division on July 14.
EOHHS has also failed to provide us records I requested on June 16 relating to a contract with Fallon Ambulance Service, which is carrying out the testing in the DDS system.
Among the records I asked for were records showing how much Fallon had been paid since they started the testing work on April 10, and copies of daily reports, which the contract requires Fallon to submit to EOHHS.
We have also have not yet received any records, which I asked for on June 25, concerning the online reporting system used by DPH regarding COVID test results in the DDS system. We want to know why the reporting system has been changed from cumulative data to current data, and why the site shows only currently positive cases.
DDS itself has provided cumulative COVID testing data to us, but the Department refuses to display the data on its website where the public could access it on a daily basis.
No indication whether administration has discussed mandatory testing
To date, no one in the administration has given us a reason for the decision not to make testing of staff mandatory in the DDS system.
On May 26, I asked EOHHS, DDS, and DPH for internal emails, memos and other records relating to internal discussions of the topic.
To date, I have received zero documents in response to my request. As a result, on July 14, I filed an appeal with the state’s Public Records Supervisor.
It’s hard to believe that there have been no such internal discussions at the highest levels in EOHHS.
EOHHS story keeps changing on the records it has
On June 9, when a response was legally due under the Public Records Law to my May 26 request for documents, an EOHHS records officer told me initial searches of emails of all EOHHS personnel using the term “mandatory testing” resulted in such a voluminous number of documents that the cost of reviewing and reproducing them would be potentially prohibitive.
As a result, I agreed to the records officer’s suggestion that I narrow the requested communications to Secretary Sudders and her executive team, and narrow the time frame to a period between April 1 and June 1, 2020.
About a month went by, and I received no further word or documents from EOHHS or from DDS or DPH. On July 9, after I queried EOHHS, the records officer said he had a “responsive record” and would provide it by July 13. When no response was forthcoming by July 14, I appealed to the Public Records Division.
The next day, the EOHHS records official emailed me to say that he had been mistaken about the responsive record, and that EOHHS actually had no records that were responsive to my narrowed request.
So, in the month and a half since my original Public Records Request, EOHHS had gone from having a voluminous number of records in response to it, to having zero records after I narrowed the request according to their suggestions.
So, I asked on July 15 if EOHHS could redirect their search to the highest-level personnel in the agency whose emails did include references to mandatory testing in the agreed-upon time frame.
Secondly, I asked for an explanation as to why it had taken more than a month since our June 9 agreement on narrowing my records request to do a search of the emails of the secretary and her team, which then came up empty. To date, I have received no response to those follow-up questions.
DPH wanted to charge us for records … then did not respond to us
On June 17, DPH responded to my May 26 Public Records request regarding mandatory testing records with a letter stating that that agency had identified more than 2,700 emails that might be responsive to my request, and that providing all of them would cost us more than $1,600.
In a June 18 email to the DPH records officer, I offered to similarly narrow my request to communications involving DPH Commissioner Monica Bharel and her executive team and to a time period from April 1 through June 1. To date, I have not received a response from DPH to my offer, nor have I received any records.
State lawmaker declines to support claim that mandatory COVID testing is prohibited by statute
In a July 7 email to a COFAR member in response to a question about mandatory testing of staff, state Representative Kay Khan stated that she has been advocating for increased testing in the DDS system.
Khan, who is House chair of the Children, Families, and Persons with Disabilities Committee, said it was her understanding, however, that requiring mandatory testing of staff is not allowed by statute and that the Massachusetts General Laws would need to be changed through legislation for this to become policy.
We at COFAR are not aware of any such statute that would prevent mandatory testing. In an email to Khan on July 8, I asked if she could provide a citation of the statute she was referring to. Khan has not responded to my query.
No new records provided regarding Fallon COVID testing contract
On June 16, I asked EOHHS for documents relating to a contract with Fallon Ambulance Service to test residents and staff in the DDS system. We had previously received the contract itself from EOHHS.
Among the documents I asked for on June 16 were records showing how much Fallon had been paid since they started the testing work on April 10, and copies of daily reports, which the contract specifically required Fallon to submit to EOHHS.
In its response on July 16, a month later, EOHHS provided only the same contract it had provided earlier. The EOHHS response stated that the agency had no daily reports from Fallon, but that we should ask DPH for those.
As far as payment to Fallon, the EOHHS response stated that I should go to the Comptroller’s online database at https://www.macomptroller.org/cthru. This database, however, does not make it clear how to determine payments made to contractors.
For instance, when I did a search for Fallon Ambulance, the Comptroller’s site appeared to indicate that the last time Fallon Ambulance was paid was in Fiscal Year 2018. When I checked it, the site listed $0 paid to the company in the previous and current fiscal years.
I emailed the EOHHS records officer about the problem with his agency’s response to my Public Records request yesterday (July 20.) I have not received a reply.
DPH ignores Public Records Request regarding its reporting system
On June 25, I asked EOHHS, DDS, and DPH for documents concerning the weekly online data reporting system used by DPH for testing results in the DDS system. We wanted to know why the reporting system had been changed from cumulative data to current data, which shows only currently positive cases.
Both DDS and EOHHS stated they would provide a response by July 17. To date, however, I haven’t received that response from either agency. I have received no communication from DPH since filing my June 25 Public Records request.
As a result, I appealed to the state Public Records Supervisor on July 16, specifically regarding the lack of response from DPH.
It’s not clear to me what, if anything, the Public Records supervisor is going to do about any of these matters.
In any event, maybe it’s just us, but is anyone else sensing a pattern here? After initially seeming responsive to our information and records requests when the viral pandemic first appeared in March, the administration has become increasingly secretive.
We are at a loss to explain this apparent lack of transparency. Overall, the administration has been getting high marks for its response to the pandemic. Massachusetts is one of the few states in the nation in which the rates of infection have been declining.
But when it comes to the DDS system, the administration just doesn’t want to answer any questions.
ACLU and SEIU surprisingly and confusingly gang up on congregate care for the developmentally disabled during COVID crisis
The American Civil Liberties Union (ACLU) and the Service Employees International Union (SEIU) are usually strong advocates of accountability and transparency in government.
That’s why it is surprising that both of those organizations appear to be using the coronavirus pandemic to further a longstanding agenda, which we never knew they shared, to privatize services to people with intellectual and developmental disabilities.
It’s particularly surprising that the SEIU, a human services employee union that represents caregivers in the state’s two remaining developmental centers, would be on board with closing down state-run care facilities.
In a petition filed June 23 with the U.S. Department of Health and Human Services (HHS), the ACLU, SEIU, and a number of other advocacy organizations appear to start off on the right track in criticizing the federal government for its mismanaged response to the pandemic.
The petition identifies nursing homes, Intermediate Care Facilities for the developmentally disabled (ICFs), and group homes as sites of large numbers of COVID-19 infections and deaths that could have been prevented with better guidance for infection control, more testing, and better patient and worker protections.
But the petition then goes on to make a number of, at times, poorly conceived and even confusing claims and recommendations that ultimately appear intended to support a privatized care agenda.
At least some of the confusion centers around group homes, which the petition lumps together with ICFs as sources of “congregate care.”
The petition suggests that among the causes of the infections and deaths is the federal government’s failure “to divert people from entering nursing homes or other congregate settings” or to increase discharges from those settings “to the community.”
The argument the petition makes is that reducing the population in all of those facilities would “make social distancing possible.”
The petition defines congregate settings as including ICFs, psychiatric facilities, and group homes. Yet, group homes are considered part of the community-based system of care in Massachusetts and other states. As a result, it isn’t clear what the ACLU and SEIU mean in stating that people living in group homes would be among those in congregate settings who should move “to the community.”
The petition, moreover, calls for reducing the population of nursing homes and congregate settings by 50 percent. Should HHS neglect to act within three weeks to enact that and other suggested measures, the groups will sue, the petition states.
It is unclear whether the ACLU and SEIU mean that nursing homes, ICFs, and group homes should all be emptied of 50 percent of their residents, or where those residents would then go.
VOR, COFAR’s national affiliate, issued a statement sharply critical of the petition, maintaining that:
…the ACLU has cast its net too wide, and falsely claimed to represent the interests of everyone receiving federally funded services who is classified as elderly or who has intellectual and developmental disabilities. In doing so, it apparently assumes that all such persons look and feel alike and need the same supports and level of care.
Further confusion over the HCBS waiver
Adding to the confusion over group homes is language in the ACLU/SEIU petition calling on HHS to “provide incentives to states to redesign their Medicaid programs to expand Home and Community Based Services (HCBS) and other community-based services and supports” with the goal of the 50 percent reduction in the population in congregate settings.
Once again, that language is confusing in that group homes in Massachusetts and other states have long been recipients of federal funding under an HCBS waiver of Medicaid regulations governing ICFs. In asking for an expansion of Medicaid funding under the HCBS waiver, is the petition suggesting that the money go toward care in a setting other than group homes?
ACLU/SEIU petition misreads the Olmstead Supreme Court decision
The ACLU/SEIU petition further misreads the landmark Olmstead v. L.C. U.S. Supreme Court decision, which paved the way for expansion of privatized care. Although the 1999 decision held that community-based care should be made available for those who desire it, it nevertheless recognized the role played by institutional care for those who can’t function under community-based care.
The Olmstead ruling stated that the Americans with Disabilities Act (ADA) “does not condone or require removing individuals from institutional settings when they are unable to benefit from, or do not desire, a community-based setting.”
We have asked the SEIU’s Massachusetts affiliate, Local 509, whether it is in support of the ACLU/SEIU petition. We have not heard back yet, but we hope they are in a position to disavow it.
There is a lot to be concerned about regarding the efforts of both the federal government and the state government here in Massachusetts to protect persons with intellectual and developmental disabilities from the virus. We’ve raised a lot of those concerns over the past few months.
At the same time, and for that reason, we don’t think it is appropriate for any organization to use the pandemic to support an anti-institutional agenda.
Baker administration now relying on provider claims, not tests, to measure COVID-19 rate in DDS group home system
Since early April, the coronavirus has been found in group homes run by more than 80% of the providers to the Department of Developmental Services (DDS), and in more than 3,400 residents and staff in the Department’s system.
Yet, according to the state’s online Weekly State Facility Reporting site, only between 7 and 12 residents are currently COVID-19 positive in the entire DDS group home system. That report stated that its data was current as of June 30.
How is it possible that the virus could have infected so many people in the system on such a widespread basis since April, and yet so few people are currently infected?
Have more than 1,300 residents alone recovered from the virus, as the weekly report claims, or is the low number of residents listed as currently positive wildly inaccurate?
It may be impossible to answer that question, given what appear to be:
- a significant slowdown since May in actual testing for the virus in the DDS system,
- an apparent reliance by DDS on reporting by the providers themselves of the number of COVID-positive residents and staff in their group homes, and the number who recovered, and
- major gaps in the data reported by both DDS and the Department of Public Health (DPH) on the incidence of COVID-19 among persons in Massachusetts with intellectual and developmental disabilities.
First, there appears to have been only a minimal level of testing done in the DDS system over the past month and a half, and virtually no on-site monitoring by DDS of the group home system. As I’ll discuss below, the downturn in testing since late May appears to correlate strongly with reporting by DDS of continuously lower numbers of new positive cases during that period.
Secondly, without the testing to determine the ongoing level of infection, DDS has apparently been relying on the providers to report accurately to it. It is unclear, however, how the providers are able to determine whether residents or staff are COVID-positive if they are not being tested.
It would seem that the most the providers can report with any degree of confidence is whether residents and staff are displaying symptoms. But as has been widely reported, asymptomatic or pre-symptomatic people can still be COVID-positive and are able to transmit the virus to others.
Thirdly, with regard to gaps in the data, the weekly state facility reports do not include the number of currently positive staff in provider-run group homes, so we have no idea what the total number of positive people in the system is right now.
The latest weekly state facility report states that as of June 30, a total of seven residents in provider-run group homes and less than five residents in state-run group homes are currently positive with COVID-19. The report also states that a total of 1,346 residents in all group homes in the DDS system had recovered from the virus. No information is given of the number of staff in provider-run group homes who are positive or the number of recovered staff.
“Recovered” individuals are defined in the reports as those who “have tested negative or have met symptom and time-based recovery guidelines issued by the the state DPH and the federal CDC.” (my emphasis).
The definition of recovered individuals appears problematic because those symptom and time-based recovery guidelines state only that a staff worker can return to work if they have been symptom-free for a total of three days. The guidelines don’t ensure that the individual is not still COVID-positive or potentially capable of transmitting the virus to others.
Nevertheless, it appears DDS has been relying more and more on reports by providers of the number of people in group homes displaying symptoms, and is no longer relying on testing to determine the number who are currently positive.
DDS has never answered our repeated question as to whether and where retesting is being done throughout the group home system. The Department also stated that it keeps no records on the number of residents reported as symptomatic. And it has no records on the number of staff who have refused testing.
Positive test numbers have closely tracked the rate of testing
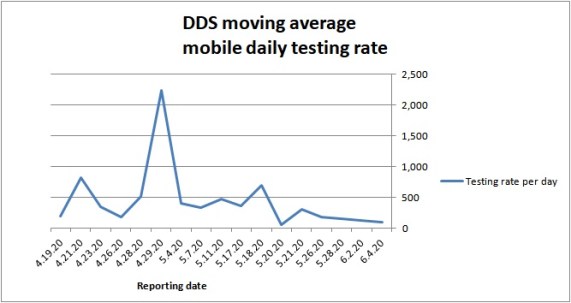
The level of mobile testing done in the DDS group home system by the state’s only contractor for that work, Fallon Ambulance Service, has slowed continuously since a peak of testing activity by the company in late April.
As of July 1, only 80 percent of the residents in the system appear to have been tested, leaving some 1,600 residents and an undetermined number of staff untested since Fallon began on April 10.
In addition, group home staff are not required to be tested and providers can refuse testing in their residences if they report that none of the residents are symptomatic.
All of those factors appear to raise questions whether the apparently declining level of positive COVID-19 cases in the group home system might not, in fact, be due to the lack of testing.
We used DDS data to show what appears to be a strong relationship between a sharply declining rate of testing for the virus since April and declining numbers reported by DDS of new positive cases among residents and staff in the system. In both cases, the numbers have trended downwards since a peak in late April or early May.
Source: DDS data reports
Both the daily rate of testing and the number of new positive cases show large spikes in late April-early May. The daily testing rate graph shows the spike occurring April 29. The positive cases graph shows the spike occurring on May 4, just five days later.
From late May onward, both graphs show lower numbers of average daily testing and positive COVID cases than had been the case in early May.
Prior to announcing a new, less restrictive policy on visitation last week, DDS Commissioner Jane Ryder stated in an email to COFAR that the number of new COVID cases “have been decreasing in DDS residential programs, much as they have across the state.” She added that DDS believed the reasons for that decline include “the visitation restrictions adopted in March…along with hand hygiene, testing, and mask use.”
Ryder didn’t note the decline in testing itself, and didn’t respond to our questions about the lower rate of testing and the possible impact it was having on the numbers of reported cases.
The administration appears to believe that if the providers are reporting fewer people showing symptoms, there isn’t a need for testing of either residents or staff. Perhaps their strategy is that if the numbers of symptomatic people start to rise, they will ramp the testing back up at that time.
In the meantime, let’s hope the providers are reporting the situation in the group homes correctly to DDS. We have no way of knowing for sure.
DDS releases provider-based data showing widespread scope of COVID-19 infections in group homes
Residents and staff have tested positive for COVID-19 in group homes in Massachusetts run by more than 80 percent of corporate providers to the Department of Developmental Services (DDS), according to data from the Department.
The data also shows that residents tested positive in all of the state-operated networks of group homes, while staff tested positive in at least three of those regional networks.
The data, which was provided last week after we had filed a Public Records request in mid-May, is the first indication of how widely the virus has spread throughout the largely provider-based DDS system.
The data also show that deaths of residents have occurred in residences operated by at least 44 corporate providers in addition to as many as three of the state-operated networks and the two developmental centers.
An undetermined number of staff have died of the virus in residences operated by three corporate-providers, although that total number is less than 15. DDS, citing privacy concerns, did not provide actual numbers in instances in which there have been less than 5 cases or deaths, but listed those as “<5” cases or deaths.
In totaling the cases and deaths, we have counted instances in the chart labeled “<5” as 1 case or 1 death, which obviously makes the totals very conservative.
For instance, while the chart shows a total of 69 deaths due to COVID-19 as of June 17, DDS has reported to us separately that the number of deaths is actually over 100. We would note that even that number may be lower than the real number of deaths due to COVID-19 because DDS has so far tested only about 75 percent of the residents in its system, and some providers have refused testing in their residences.
The chart is based on cumulative provider-based information reported to DDS as of June 17. We have ranked the providers from highest to lowest in the reported number of positive COVID-19 cases among residents of the facilities.
You can also download this DDS COVID-19 provider breakdown spreadsheet.

The data shows positive cases occurring among residents in group homes operated by at least 103 of 125 DDS corporate providers, or 82 percent of them. It also shows positive cases among staff in residences operated by at least 111 providers, or 88 percent.
A total of 22 providers reported zero positive cases among residents. However, it could be that at last some of those providers have not allowed any testing in their residences. DDS has provided separate data to us stating that since April, 1,100 out of a total of 2,100 provider-run group homes reported positive cases in those residences.
As the chart above also shows, there have been 5 deaths reported at the Hogan Regional Center, and at least one death reported at the Wrentham Regional Center as of June 17. There have also been at least one death each in networks of group homes operated by 44 out of 125 corporate providers, and by 3 or more of the state-operated networks.
Caution in interpreting the data
We would offer some words of caution in interpreting this data. One is that it is based on reporting by the providers themselves to DDS, and it is also based on what has so far been a limited amount of testing done of residents and staff. As noted, if a provider has zero positive cases on the list (as the blank cells indicate), that could mean that they are among the providers that have refused testing, claiming that no one in their group homes has shown symptoms.
Similarly, if a provider or group home network is ranked high on the list, that may not necessarily mean conditions are more dangerous in those residences. Northeast Residential Services (NRS), a state-operated group home network, is at the top of the list in the number of residents testing positive, with 82 residents and 73 state-employee staff testing positive. However, NRS is also one of the largest networks of group homes in the state.
We also know that residents have been repeatedly retested in NRS homes. It is unclear whether residents are subjected to retesting in corporate provider-based homes. We have never gotten an answer from DDS to our question whether retesting is done in more than a small number of provider residences.
Among providers, Vinfen, also one of the largest corporate DDS providers, is second highest in the number of positive cases among residents, with 78 residents and 64 staff testing positive. Bridgewell, another large provider, had 100 staff testing positive — the highest number of positive staff on the list.
As the chart shows, as of June 17, there were at least 1,520 positive total cases of the virus among residents, as reported by the providers and by the state-operated group homes, and two state-run developmental centers.
There have been at least 1,355 corporate provider staff testing positive, and at least 401 state-employee staff testing positive. (This is the first breakdown we have had of the number of corporate provider versus state-employee staff testing positive.)
NRS has had the highest number of deaths, with 10 in its group home network. Vinfen is second highest, with 8 deaths in its residences.
It’s not possible to tell from the data provided which group homes the positive cases or deaths have occurred in, or when these cases occurred.
It was notable, but not surprising, that the DDS response to our May Public Records Request stated that the Department does not have records on the number of residents showing symptoms or the number of staff refusing to be tested. We had asked for those records as well. It’s further evidence that the DDS data collection system has big gaps in it.
We would point out that this provider breakdown of COVID-19 testing data is information that a number of families in the DDS residential system have apparently asked for, but which the Baker administration has so far refused to publish online.
Information has long been available on the state’s website about COVID-19 cases and deaths in nursing homes and other long-term care facilities overseen by Department of Public Health (DPH), and even in correctional facilities. But no such detailed information is posted about DDS providers.
It took DDS more than five weeks to respond to our Public Records request for the breakdown of the testing information by provider, necessitating an appeal by us to the state Public Records Supervisor.
We will continue to ask DDS for updated information on COVID testing, broken down by provider. It still appears that we will have to either ask the Department on a periodic basis for this information or file further Public Records requests in order to obtain the latest data.
If DDS does not provide the information in a timely manner, we are reserving our rights to renew our appeal for those records.
A comparison of two contracts for COVID-19 testing shows a bias against persons with developmental disabilities
We examined two emergency contracts that the state has signed with two separate ambulance companies to test different groups of people for COVID-19 in congregate settings.
The comparison of the two no-bid contracts provides yet more evidence that the administration is less concerned about persons with intellectual and other developmental disabilities than it is about other populations.
We received both contracts from the Executive Office of Health and Human Services (EOHHS), under a Public Records Law request.
One of the contracts, signed with the Quincy-based Fallon Ambulance Service, is for testing residents and staff in group homes and developmental centers funded by the Department of Developmental Services (DDS.) The contract doesn’t mention DDS, however, which is part of the problem.
The other contract, with Weymouth-based Brewster Ambulance Service, is to test persons in nursing homes and other congregate facilities for the aged, many of which are licensed and regulated by the Department of Public Health (DPH). The contract appears technically to be an amendment to an existing contract between Brewster and EOHHS.
Lack of specifications
To start with, the Fallon contract doesn’t specify testing at DDS sites, and, as noted, doesn’t mention DDS. It says only that Fallon must “travel to sites as specifically directed by EOHHS” and test “certain individuals” for COVID-19. The contract doesn’t specify that Fallon must test either residents or staff.
DDS has told us that Fallon’s job is ultimately to test all residents and staff in the group homes and developmental centers in its system, and that Fallon is the only company currently undertaking that testing service for DDS.
The Brewster contract, in contrast, specifies that the company must test for COVID-19 in skilled nursing facilities, assisted living, rest homes, and senior housing. That contract also doesn’t specify testing of residents or staff, but the administration has required that the facilities test all staff in order to receive hundreds of millions of dollars in funding for COVID-related costs.
We have reported that staff in the DDS system, on the other hand, can opt out of testing altogether, and the Fallon contract appears to reflect that situation.
In not specifying DDS facilities, the Fallon contract casts doubt on the state’s commitment to fully test individuals in the DDS system.
No minimum daily amount of testing required
Despite the emergency nature of the COVID crisis and the emergency procurement of the Fallon services, there is no sense of emergency in the terms of the contract itself. There is no required daily rate of testing, for instance, and no timeline for testing the entire DDS system.
There is no timeline in the Brewster contract either, but that contract does require testing a minimum of 250 individuals a day, 7 days a week, and requires that the company communicate results of tests within 72 hours to those tested.
As we have reported, Fallon’s testing rate has been steadily dropping. Between June 1 and June 15, Fallon has averaged only 80 tests a day, according to DDS data. That is down from a peak on April 29, when the company performed more than 2,000 tests on that one day.
To date, based on the data, Fallon has tested about 75% of the total residents in the DDS system, leaving more than 2,000 residents and an undetermined number of staff waiting for their first test.
The Brewster contract requires the company to “prioritize” its testing services under the contract “over the provision of identical or similar services for any other entity to which it provides services.” There is no similar provision in the Fallon contract.
Contract was not signed until weeks after Fallon started
Although Fallon began testing in DDS residential facilities on April 10, according to the Department, the Fallon contract was not signed until May 19 by a Fallon senior vice president, and until May 27 by a top EOHHS official.
Thus, Fallon was doing the testing for more than six weeks before the contract was signed by both parties to it.
The contract states that it is effective from April 7 through December 31, or 60 days after the expiration of the state of emergency, whichever is earlier.
Leaving aside the legal implications of not signing the contract, the fact that the state, in particular, didn’t bother to sign it for six weeks, raises further questions about the administration’s commitment to testing in the DDS system.
Even if the contract had provisions requiring Fallon to test at a minimum rate, the state would have had no legal means of compelling the company to meet such requirements if there was no signed contract.
The Brewster contract was signed on May 4, the date that the company began working under the EOHHS testing program, according to the contract.
We first asked EOHHS for the Fallon contract on May 21, but it apparently hadn’t yet been signed by both parties to it. We didn’t receive the two contracts from EOHHS until June 15.
Both contracts contain detailed requirements regarding testing procedures, the use of Personal Protective Equipment by testing personnel, and the use of certified labs that analyze the results. The fact that no such provisions were in effect contractually in Fallon’s case for six weeks raises questions about the nature of any agreements that EOHHS had with the provider to follow testing protocols and use certified labs.
No projected total contract payment
Neither the Fallon nor Brewster contracts project a total payment amount, and each contract specifies a different level of payment per testing visit.
The Fallon contract specifies payment of $80 per hour for each EMS personnel. The testing team consists of two EMS personnel, a “tech” and a “monitor.” The contract does not appear to be clear about payment of the tech and monitor.
The Fallon contract also specifies that the company will be paid for one hour prior to the beginning of each testing visit and one hour after completion to cover planning, travel, and other tasks.
The Brewster contract refers to an administrative executive order (Administrative Bulletin 20-18), which appears to specify a flat payment of $305 per testing visit.
New contract needed for DDS testing
“It sounds like it (the DDS testing) is ending in the manner it began – an empty husk,” said COFAR President Thomas Frain. “If you apply the same criteria to DDS testing that are on display for everyone else, i.e. the importance of testing in keeping people safe, this has been a failure.
“People challenged by intellectual disabilities are treated disparately,” Frain continued. “We were made promises about testing of our loved ones that have turned out to be false and (EOHHS) Secretary (Marylou) Sudders and DPH are in the thick of it.”
Sudders, in particular, never responded to our email query in May as to why Fallon’s daily testing rate was so low in the DDS system and why no other company had been hired to supplement Fallon’s testing efforts.
We think a new contract needs to be drafted that specifies testing of residents and staff in the DDS system and sets a minimum daily testing rate that is significantly higher than what Fallon is currently doing. Moreover, DDS should seek competitive bids for that contract.
Onerous and inconsistent restrictions placed in some cases on families in post-COVID-lockdown visits
Limited visits by family members to loved ones in the Department of Developmental Services (DDS) residential system began last week, technically ending the COVID-19 lockdown.
But we have gotten reports that some of the restrictions placed on those visits have been onerous and others inconsistently applied.
While some families have reported that their first visits went very well, others have had problems. There appears to be a lack of consistency in how different providers are treating the same types of situations.
On Monday, COFAR Executive Director Colleen Lutkevich and President Thomas Frain sent an email to DDS Commissioner Jane Ryder, pointing out concerns about the process, and about highly restrictive DDS visitation guidelines that the Department issued last week to families.
When we first read the visitation guidelines, we were immediately concerned that their restrictive nature and the large amount of discretion given to providers might result in inappropriate or unnecessary bans on family contact.
We are also concerned that at the same time that DDS has begun allowing family visitation, the Department appears unconcerned that the rate of testing in the residential system for the virus has slowed down to a practical standstill.
During this past week, we have received reports that appear to bear out our concerns about the visitation restrictions.
In one case, a parent said she was told she cannot visit her son, who she hasn’t seen since the lockdown began in March, because some of the residents in his group home had tested positive after being retested. Because her son has consistently tested negative, she asked the provider if her son could have an off-site visit with her, but her request was denied. She said the provider told her DDS has forbidden off-site visits.
That reported statement by the group home provider about off-site visits appears to contradict DDS’s position as we understand it. On June 8, DDS Ombudsman Christopher Klaskin stated to us in an email that even prior to the resumption of the currently limited visitation, “group homes were not fully locked down, enabling providers to take individuals for walks or even on short outings (to parks, drive through restaurants).”
It doesn’t make sense to us that even during the lockdown, residents were taken off site to commercial establishments in which they presumably were brought into proximity with strangers who may or may not have been wearing masks. Yet now, during a resumption of family visitation, residents are not allowed to have off-site visits with their families, and some providers are not allowing family members to take residents off site even to parks or places free of other people.
Given that off-site visits to commercial establishments have been allowed all along, off-site visits with family members should be permitted as well, Frain and Lutkevich stated in their email to Ryder.
In one case, a parent got mixed messages from two different supervisors in her son’s group home. One supervisor said she could not walk with her son on the sidewalk in front of the house, while another supervisor said she could do that. She said she would love to drive her son to a park to walk, but was told she is not allowed to take him in her car.
Meanwhile, another parent said the staff of a group home took his daughter and another resident out for “a very long walk around a scenic park next to the home.”
Another parent said that prior to the lockdown in March, her daughter was used to coming home every weekend, “and is emotionally getting affected at this point severely.” She added that not only is her daughter not allowed to come home even now, “they (the group home staff) aren’t even doing outings.”
The mother of a resident at the Hogan Regional Center said she had been scheduled to visit her son on June 10 for a half hour outside with masks on. But she received a call and email the night before informing her that the visit was put on hold because a resident in a different building had tested positive for COVID-19, and that all visits were on hold.
The woman then asked if her son could be allowed out on the screened porch in his wheelchair at the facility while she stood outside on the lawn “just to see him and him hear my voice.” She was told that was not allowed.
Another parent told us her child has not had a hug and most likely little to no human touch since mid-March. She was told by her provider that she cannot bring a birthday cake to share with her daughter even while they are outside and 6 feet apart.
The woman in that case said she offered to stay 15 feet away while eating, but was told that was not allowable because she and her daughter would have to remove their masks to eat. Yet, during the lockdown, the same provider was taking the woman’s daughter to fast food restaurants and other commercial establishments.
Lutkevich and Frain suggested that DDS send guidance to the providers on how to handle the resumption of visitation. They noted that DDS has sent very restrictive guidelines only to families.
“Given the discretion that the providers have under those guidelines, we think the providers actually need to be told that families should be treated with respect in these circumstances,” Lutkevich and Frain stated.
Lutkevich and Frain added that the types of apparent inconsistencies in restrictions they described “need to be addressed, and common sense needs to prevail.”
For instance, they said, providers need to be told that families are allowed to take their loved ones off site if it can be done safely. That appears to be DDS’s position, as we understand it, but some providers apparently don’t seem to know that.
What this all seems to highlight is an ongoing pattern in which DDS places burdens on families in the stated interest of furthering the safety of the residents while avoiding anything that can be seen as burdensome on providers.
Why place difficult restrictions on visits by families to group homes while, at the same time, failing to ensure that timely testing for the virus is taking place in those facilities? What purpose does it serve other than prolonging the suffering that people have been enduring for months now?
DDS allows strictly controlled family visitation even as it relaxes COVID-19 testing requirements on providers
As Governor Baker continues to reopen the state’s economy due to declining rates of infection in the general population from the coronavirus, the Department of Developmental Services (DDS) announced it is allowing strictly controlled visitation by family members and guardians of loved ones in its residential system.
Yet at the same time, DDS appears to be reducing its levels of testing of individuals for COVID-19 in its group homes.
We strongly support the resumption of family visits. But we are concerned about the apparent lack of consistency by DDS in relaxing testing of residents and staff as the homes are being opened to visitors after a lockdown since March.
The numbers of positive tests for DDS residents are continuing to climb, and the number of deaths in the system, while still relatively low, have been rising as well.
At this critical juncture, DDS appears to be making life difficult for families and easy for providers. The new visitation rules appear not only to have onerous provisions, they contain multiple threats that visits will be terminated and family members banned from any further visits if the providers determine they are in violation of any of the provisions.
Under the new visitation rules, which go into effect tomorrow (June 10), the duration and nature of family visits will be sharply limited, and providers will have discretion to set the terms for the visits and to ban families for perceived violations.
But if DDS is so concerned about family members violating its restrictive visitation policies, the Department does not appear to be concerned that:
- An undetermined number of providers have decided that there will be no COVID-19 testing in their group homes
- Testing of staff continues to be voluntary
- The pace of mobile testing of the group home system appears to be slowing almost to a standstill
- Retesting of individuals appears to be sporadic at best or nonexistent at worst.
Last week, I emailed Christopher Klaskin, the DDS ombudsman, asking whether DDS remains committed to testing the entire group home system, or whether the Department believes that universal testing of residents and staff is not necessary or no longer necessary.
Klaskin did not respond to the question. He did say that DDS is currently “educating providers on the importance of testing and how that data ultimately will inform how we proceed in the phased reopening of our facilities.”
The declining rate of DDS COVID-19 testing may reflect a drop in the rate of testing of the population of the state as a whole. The Boston Globe reported yesterday that even as the administration is opening up businesses throughout the state, COVID-19 testing has dropped to the lowest rate in months.
Testing that has been done by DDS shows that the number of persons in the residential system is continuing to rise (see graph below), and the rate of DDS residents testing positive remains higher than general population. The death rate in the DDS system is still low, but deaths are still rising.
Given the factors noted above about the testing rate and requirements, the positive infection rates in DDS group homes may be higher than the DDS data show.
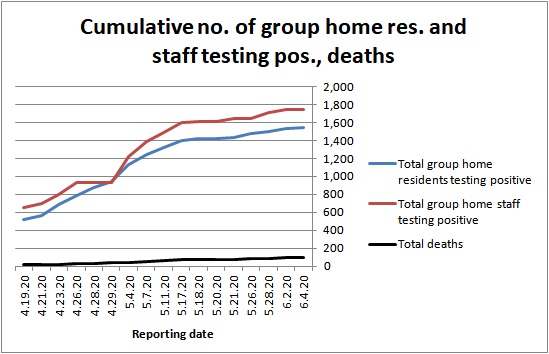
Source: DDS
Testing rate appears to be slowing
Fallon Ambulance Service, which started mobile testing of the DDS residential system on April 10, has tested only 72% of residents and staff in group homes. More than 2,000 residents have yet to be tested.
As the chart below shows, the daily testing rate by Fallon is actually down to less than 200 tests a day. The overall average daily rate since Fallon started on April 10 is 438. But that average is driven by a large spike of tests on April 29, when Fallon actually did more than 2,200 tests.
While Fallon is apparently capable of doing more than 2,000 tests per day, they haven’t done anywhere near that amount per day since the end of April.
Source: DDS
We filed a Public Records Request with the state last month for Fallon’s contract and related procurement documents. The Executive Office of Health and Human Services has asked for an extension until June 12 to provide those documents.
We have expressed concerns for some time about the slow pace of Fallon’s testing, and have gotten no response from Health and Human Services Secretary Marylou Sudders as to why no additional companies have been hired to supplement Fallon’s work.
DDS says it isn’t requiring testing of all group homes
Also concerning to us is that DDS has acknowledged for the first time that not all provider residences are being tested for residents and staff who might be infected with the virus. This appears to violate DDS guidance and previous statements made by the Department.
I asked DDS ombudsman Christopher Klaskin last week about the matter after we heard from a parent of a resident of a provider-run group home who said she was informed that no one in the home had been tested because no one was symptomatic, and that the provider did not intend to implement mobile testing in its residences.
DDS guidance, which was sent in April to all providers states that the intent of the Department’s mobile testing program is to “have all individuals and staff tested,” and that those that are symptomatic would be “prioritized.” (my emphasis). That is also the message that DDS Commissioner Jane Ryder gave us when we talked with her in a conference call in April.
On Friday, Klaskin confirmed that “some locations have not requested testing” if staff or residents have not been symptomatic. Klaskin said that in those cases, DDS has told the providers that all residents and staff need to be continuously monitored and that they must request mobile testing or another means of testing “as soon as an individual shows symptoms or has been exposed to the virus.”
DDS’s written guidance, however, doesn’t state that testing will be done only if providers request it, or that asymptomatic residents can be monitored rather than tested. The guidance specifically states the Department’s intent is to test all individuals and staff.
It appears providers can avoid testing altogether by stipulating to DDS that no one in their residences is symptomatic. Thus far, 52% of provider-operated homes have reported positive cases to DDS, according to departmental data; so the remaining 48% could conceivably decline testing. We have asked DDS for the number of homes that have declined all testing.
Retesting may be being done only in ICFs and state-operated group homes
The issue of retesting of residents in the DDS system is critically important in ensuring that the true rate of infection over time is known and controlled. However, the amount of retesting that is being done in the system is unknown, and the nature of any retesting that is being done appears to be sporadic at best.
In April, when we first asked about the issue, Klaskin implied that DDS was not doing any retesting. In an email on April 20, in response to a question about the issue, Klaskin wrote, “DDS and Fallon are currently focused on testing all facilities before mobile retesting can be made available.”
Early this month, however, we began to receive reports that Fallon was actually returning to some state-operated group homes to retest residents there who had previously been tested. When I asked Klaskin about that and specifically asked where the retesting was being done, Klaskin said only that Fallon “has increased their capacity to now retest locations meeting CDC criteria for retesting.”
Klaskin didn’t respond to my questions where the retesting was being done or why some residents were being retested while others were still waiting to be tested for the first time.
Family members singled out for visitation restrictions
In light of the decision to loosen a virtually complete ban on visitation, DDS issued new guidelines on June 6. But those guidelines appear to be harder on families than the COVID-related requirements DDS is imposing on the providers themselves.
Under the new rules, families will not be allowed inside the residences for any reason. Residents are limited to two visitors at a time, and providers have discretion to limit the number of visits, times per week, and length of visits.
At the same time, the guidance says visits will be limited to a maximum of once a week and 30 minutes. Failure to adhere may result in a “termination of the visit” and a “temporary ban” on visits. DDS or providers can change the policy with “little notice,” and providers can also prohibit visits if they determine for any reason that the visits are not safe.
We have seen many cases in which providers have banned family members and even guardians from visiting loved ones on the basis of flimsy pretexts.
Yet despite the virtual ban since March on visits, and the severity of the restrictions even now, one parent said her daughter has been taken out by staff during the lockdown to commercial establishments and fast food restaurants.
There appears to be little consistency in DDS’s response to the ongoing coronavirus crisis. Even as the Department is opening up the residential system to visitors, it is slowing down the COVID-19 testing rate and allowing providers to avoid testing altogether if they stipulate that no one is symptomatic.
DDS officials will not even commit publicly to the clear statement in their guidance that all residents and staff in the system should be tested.
And despite the relaxed attitude DDS has adopted toward testing for the spread of the virus in the group home system, in particular, it is maintaining harsh restrictions on family visitation and giving providers the discretion to ban family members from residences for any perceived violations.
We think DDS needs to rethink both of those stances. The Department should recommit itself to universal testing in its system; and it should not give providers complete discretion to ban families from visits for perceived violations of overly onerous restrictions.
DDS residents have tested positive for COVID-19 at higher rate than general population
Residents with intellectual and other developmental disabilities in group homes have tested positive for COVID-19 at a significantly higher rate than the general population in Massachusetts since the end of April, according to an analysis by COFAR.
The numbers appear to demonstrate the importance of maintaining safe conditions in the homes and testing all staff, particularly if the administration begins to loosen lockdown restrictions in coming weeks.
COFAR analyzed cumulative testing data provided by both the Department of Developmental Services (DDS) and the Department of Public Health (DPH). DDS tracks testing data for residents and staff in its residential facilities, and DPH tracks and publishes testing data for the general population on a daily basis.
COFAR found that on a cumulative basis, the COVID-19 positive rate of DDS residents was 18.4% between April 23 and May 26, while the positive rate in the general population was 12.5% during that same period. That’s a 47% higher positive rate for DDS residents.
While the high rate of COVID-19 infection in nursing homes is widely known, it hasn’t been reported in the media in Massachusetts that residents of DDS group homes have apparently also contracted the virus at a higher rate than the general population.
The number of deaths in DDS group homes has been lower on a percentage basis than in nursing homes, but that death toll is continuing to rise. As of May 28, there have been 87 deaths in the DDS system, up from 78 deaths ten days earlier.
It is not clear why the death toll has been relatively low in the DDS system. But it should not come as a surprise that the conditions that have caused the quick spread of the virus through nursing homes are similar to those that exist in DDS-funded group homes.
Group homes are small, household sized facilities in which DDS residents have been locked down since March. As such, a virus can spread quickly in a group home especially if it is introduced by an outside source — namely staff who are, in many cases, not being tested.
COFAR tracked cumulative DDS and DPH testing data within a period from April 23 through May 26. DPH publishes testing data on a daily basis and breaks it down among several demographic categories.
The general population data that COFAR analyzed is contained in this linked DPH report, which is referred to as the DPH “COVID-19 Dashboard,” and is updated and published daily by that agency.
But the DPH report does not break out data for persons with intellectual and developmental disabilities. COFAR has obtained testing data on persons in the DDS system after directly contacting DDS on a daily basis.
We compared DDS and DPH testing data after April 23 because that was the first date for which we received data from DDS showing the total number of residents tested in the system. The state engaged Fallon Ambulance Service on April 10 to begin testing residents and staff in group homes and at the Wrentham and Hogan developmental centers.
Starting April 10, DDS began reporting results on positive tests on a cumulative basis. DPH has, in contrast, reported test results and test numbers on a daily basis; so we added the DPH daily testing numbers together since April 23 in order to make the numbers from both agencies comparable.
In the period between April 23 and May 26, Fallon Ambulance Service tested a total of 4,500 residents in both DDS group homes and the two developmental centers. During that time, 826 DDS residents tested positive, according to the DDS data. That appears to be a cumulative positive test rate of 18.4%.
During that same period, the DPH website document linked above shows that 320,243 members of the general population were tested in Massachusetts, and that of that number, 39,928 had tested positive — a cumulative positive test rate of 12.5%.
(Note: DDS ombudsman Christopher Klaskin maintained that the numbers provided by DDS of residents testing positive include the results of tests done by sources in addition to Fallon, whereas the total numbers of tests done reflect only those tests done by Fallon since April 10. As a result, he maintained, the numbers provided by DDS of persons testing positive cannot be compared to the numbers provided of tests done.
Klaskin said DDS doesn’t track either the number of positive results from tests done by sources other than Fallon or the number of tests done by those other sources.
As a result of Klaskin’s assertions, we limited our comparison to tests done after April 23, the date for which we first got a breakdown from DDS on the total number of residents tested. We do not think it is likely that more than a negligible number of tests have been done in the DDS group home system outside of Fallon’s mobile testing process.)
Governor, planning to restore visitation, cites declining positive test rate
According to the State House News Service, Gov. Charlie Baker said last week that COVID-19 public health data indicates “that we are trending in the right direction.” As a result, the head of the state’s COVID-19 Command Center said plans are in the works to allow people to once again visit their loved ones in long-term care settings.
Residential facilities in the DDS system have been locked down, with few visitors permitted to enter them since March. DDS group home licensure inspections have been discontinued as well.
In that light, we are urging that the administration take measures to better ensure the safety of the residents in DDS facilities. We think DDS can start in that direction by making testing of staff mandatory.
Disability Law Center echoes our concerns on staff testing and safety
A May 21 letter from the Disability Law Center in Massachusetts, a partially federally funded nonprofit organization, echoes many of the concerns COFAR has raised with regard to testing and safety conditions in the DDS system.
The DLC letter to Dan Tsai, assistant secretary for MassHealth, calls for mandatory testing of staff in the DDS system, better training of staff in using Personal Protective Equipment in group homes, and better reporting of data by DPH.
The DLC letter adds that there is still no “firm rule” which prevents direct support staff from working for multiple employers in different DDS group home settings. The letter also notes that the waiting period for previously COVID-positive staff to return to work is seven days, whereas the public health standard is 14 days.
Also, according to the letter, there are no “clearly enforced protocols” against DDS-funded staff working with COVID-positive and COVID-negative residents within the same shift. COVID-positive and COVID-negative residents “are being confined together in close quarters within group homes, often with COVID-egative residents getting little or no fresh air,” the letter stated.
The DLC letter stated that there is a lack of “strong protocols” for testing, screening, and separating transportation providers, such as van drivers, who may be COVID-positive.
The letter added that to the extent that there may be legal barriers to imposing additional safety requirements on providers, such as mandatory testing, those barriers may be overcome through DPH’s emergency powers or DDS’s ability to adopt emergency regulations, as many other jurisdictions have done.
Secretary Sudders still has not responded to us
Meanwhile, the pace of testing remains slow in the DDS system. Health and Human Services Secretary Marylou Sudders has not responded to our question, emailed to her on May 20, why only one company, Fallon Ambulance Service, is being used to do the testing.
Moreover, we received reports this past weekend that while thousands of residents are still waiting for their first COVID-19 test, residents in some group homes were being retested on a regular basis.
We have asked DDS for an explanation of the testing sequence in the group home system.
In sum, the DDS group home system remains a potential tinderbox that still could erupt if additional safety precautions are not taken. The higher-than-average COVID-positive rate of residents in the system over the past month is evidence of that potential.
It is unfortunate that at this critical juncture in the COVID-19 crisis, in which the administration is considering loosening many of the restrictions that have kept the crisis under control, top administration officials appear to lack accountability.
It is unconscionable that Health and Human Services Secretary Sudders does not feel it necessary even to respond to basic questions about the testing process for residents and staff in the DDS system.
The administration needs to do a better job of ensuring the safety of clients of the DDS system and of demonstrating to families and the public in general that it is in control of the situation.
Administration mum so far on why DDS COVID-19 testing process has been so slow
Although we have been getting data and responses from the Department of Developmental Services (DDS) to questions about COVID-19 testing results in group homes, no one in the administration is saying why the testing has been going slower than projected, and no one seems concerned about speeding it up.
According to the latest data we have from DDS, which was as of Thursday (May 21), the Department’s mobile testing provider, Fallon Ambulance Service, had tested 16,200 residents and staff, most of them in group homes throughout the system.
While that may sound like a lot, Fallon, a Quincy-based company, began testing on April 10, and has been averaging under 400 tests per day since then. DDS Commissioner Jane Ryder stated early on that Fallon had the capacity to perform up to 1,000 tests per day.
At this point, six weeks into the testing program, Fallon has tested about 65% of what we had estimated to be a total of 25,000 residents and staff in the DDS system. As we understand it, there has been no retesting of any of those persons living or working in the group homes, although we have heard that some people have been periodically retested in the Wentham and Hogan developmental centers.
Our estimate of the total number of staff in the DDS system might be low. WCVB Channel 5 news reported last night that there are a total of 34,000 staff working in the DDS system. If that is the case, Fallon has tested only 35% of the total number of residents and staff in the system.
The number of residents tested, in fact, stayed the same between Monday (May 18) and Wednesday. As of Monday, 5,600 residents and 10,200 staff had been tested throughout the DDS system.
As of Wednesday (May 20), DDS data showed the number of residents tested had remained at that same 5,600 level, while 100 additional staff had been tested. It would appear from those numbers that between Monday and Wednesday of this week, Fallon was averaging only 50 tests a day, and the company tested only staff during that time.
Despite the slow pace, the actual results of the testing continue to be important and concerning. More than 3,300 of the total staff and residents tested — or nearly 21% — have been found to have COVID-19. And the DDS data shows that more than 50% of the provider-run group homes in the state have now reported cases of the virus in their residences.
That data only underscores the importance of conducting the testing on a more timely basis.
We first raised a concern about the apparently slow pace of the testing process about a month ago. We also expressed a concern at that time — the first of many times since — that the testing process was voluntary for staff in the group homes. Apparently little or nothing has been by the administration to address either of those concerns.
Neither DDS or EHS commenting so far on the slow pace of testing
When we got the data from DDS that as of Monday, only 15,800 persons in the DDS system had been tested, I emailed DDS Ombudsman Christopher Klaskin to ask if Fallon was still the only company doing the testing. We heard reports that at least one other ambulance company was interested in supplementing the testing done by Fallon.
Klaskin wrote back to me on Wednesday, stating that Fallon “is the only provider contracted to perform mobile testing for DDS and several other EHS (Executive Office of Health and Human Services) agencies.”
Given that Fallon had by Monday been on the testing job for 39 days and was thus averaging only 405 tests a day since starting, I asked Klaskin whether any other companies had expressed interest in supplementing the testing, and why Fallon was still the only company doing the work. Klaskin declined to respond to those questions, saying Fallon is contracting for the work with MassHealth, which is part of EHS, and that I should direct my questions to them.
So, on Wednesday afternoon, I emailed EHS Secretary Marylou Sudders with essentially the same questions, and asked whether the state was seeking to contract with any additional companies to undertake the testing. Thus far, I haven’t gotten a response either from Sudders or from Jessica Lyons, the communications manager for MassHealth, whom I had also emailed on Wednesday.
Also on Wednesday, I filed a Public Records request with EHS/MassHealth and DDS, asking for the contract with Fallon for testing in the DDS system, and any related procurement documents and memoranda that address the need for the procurement, the scope of the services, the projected costs, timelines, and capacity of the company, and any applications filed by any other companies to undertake or supplement the testing program.
Testing is a critically important part of the process of getting us through the pandemic with as little additional loss of life as possible. The Baker administration has made testing a priority, and Massachusetts has, in fact, acquired a reputation as a leading state with regard to testing its residents overall.
But when it comes to ensuring the speediness and thoroughness of testing of persons with intellectual and other developmental disabilities and their caregivers, the state has once again fallen short. And no one in the administration appears to be willing to acknowledge or discuss it.
DDS may be flouting state and federal guidelines in failing to make testing of group home staff mandatory
While testing of staff for COVID-19 remains voluntary in group homes funded by the Department of Developmental Services (DDS), state guidelines appear to require testing of staff in small facilities in which at least some individuals are symptomatic.
Meanwhile, a state senator, who filed a bill (S.2657) to make testing of staff mandatory in nursing homes, is reportedly supporting mandatory staff testing in the DDS system as well. A legislative aide to Senator Jamie Eldridge said Eldridge supports amending his bill to make testing mandatory for DDS group home staff.
Eldridge’s legislative aide said he notified the Legislature’s Public Health Committee of the senator’s support for that change. Eldridge’s bill is currently in the committee.
While DDS started a mobile program more than a month ago to offer tests to every resident and staff member in its residential system, DDS has stated that the tests are voluntary for staff. In addition, DDS has no current plans to undertake periodic re-testing of either residents or staff.
We have repeatedly raised the concern that staff are potentially the main source of introduction of the virus to group homes, in which residents have been locked down from nearly all visitation since mid-March.
As a result, even as the rate of COVID-19 cases among all residents of the state has started to taper off and Governor Baker has introduced a detailed plan to reopen the state’s economy, the number of COVID-19 cases in the DDS system appears to be continuing to rise rapidly.
As of May 11, the last day for which DDS provided data to us, 1,000 provider-run homes in the DDS system were reporting positive COVID-19 cases. That is nearly 50% of the total number of provider-run homes in the system, and that was up from 900 homes reporting positive cases as of May 7. We are asking DDS for more up-to-date figures.
Despite the voluntary nature of the staff testing in the DDS system, COVID-19 testing guidelines from the Department of Public Health (DPH), dated May 13, state that “all individuals” who have “close contact” with persons showing symptoms “should be tested” for COVID-19.
Under DDS’s own guidelines, group homes appear to be a type of facility in which close contact is unavoidable. Those guidelines define “close contact” as “living in the same household as a person who has tested positive for COVID-19, caring for a person who has tested positive for COVID-19, or being within 6 feet of a person who has tested positive for COVID-19 for about 15 minutes.”
As a result, the DPH guidelines would seem to require that all staff be tested if they are working at least in those group homes in which one or more residents are symptomatic.
Also, guidelines from the federal Centers for Disease Control (CDC) identify “workers in congregate living settings” as a “high priority” for testing if they themselves have symptoms of COVID-19. Other persons in that high-priority class, if they have symptoms, are residents in those facilities and hospitalized patients.
DDS, however, is not requiring group home providers to test staff even if the workers have symptoms. While those staff are precluded from working in the residences while they are ill, they can return to work three days after recovering from their illness without necessarily getting tested.
Guidelines have some apparent contradictions regarding staff testing
Despite the clear-sounding statements in the guidelines regarding staff testing, DDS may consider that it has some leeway in complying with those statements because some seemingly contradictory language can also be found in those same documents.
For instance, while the DPH guidelines state, as noted, that anyone in a residence who has close contact with a symptomatic individual should be tested, the same guidelines also contain the following statement:
Asymptomatic individuals can be recommended for diagnostic testing at the discretion of their healthcare provider, a state agency, or an employer. Individuals are encouraged to confirm with their insurance whether the test will be covered. (My emphasis)
That language in the latest DPH guidance seems to directly contradict the previously noted language in the same document that states that “all individuals” having close contact with persons who are symptomatic “should be tested.”
Meanwhile, despite the CDC’s guidelines that refer to staff with symptoms as a “high priority” for testing, another set of CDC guidelines allows infected healthcare staff to return to work without necessarily getting tested. Those latter guidelines and guidelines from the Baker administration’s COVID Command Center both appear to leave it to the discretion of the provider or individual state agencies as to whether to re-test staff returning to work after they have recovered.
Both the CDC and the state COVID Command Center refer to “test-based” and “symptom-based” strategies for returning to work.
Guidance sent by DDS last month to all group homes appears to adopt the “symptom-based strategy” for allowing a staff worker who has COVID-19 symptoms to return to work after they have recovered without being tested. Under the DDS guidance, that worker would be prohibited from working in the group home for three days after recovering from the illness. If the staff worker were to be tested at any point and the test was positive, that worker would be excluded from work for seven days from the date of the test as long as the worker showed no symptoms.
In neither of those cases does the DDS guidance require testing or re-testing for COVID-19 before that worker can return to the group home or to one of the state’s two developmental centers.
DDS has stated that “very few” staff have so far refused to cooperate with the testing program; however, we have received a number of reports from family members of some group home residents that none of the staff in those homes, or very few of them, were being tested.
The situation is different in nursing homes in which staff testing is required if the nursing homes want to receive grant money made available last month by the administration.
DDS Ombudsman Christopher Klaskin maintained last week that DDS “continues to follow the CDC and DPH (state Department of Public Health) guidance for testing in our group homes.”
Klaskin added that both the CDC and DPH “differentiate between nursing facilities (which are health care facilities) and congregate care settings (like group homes), so operational protocols issued for these two systems are different.”
In our view, however, the CDC guidelines do not appear to differentiate between healthcare facilities and congregate care settings, but rather state that workers in both types of facilities either are or potentially are priorities for COVID-19 testing.
As a result, I wrote to Klaskin on May 13, asking why DDS does not at least require re-testing of group home staff before returning to work after those persons have previously tested positive or had symptoms.
In a related development, we have written to the chairs of the House and Senate Ways and Means Committees and to a key senator, asking for a change in a separate bill (S.2695) that would require DPH to publicly report testing data on residents and staff in DDS group homes.
The bill, as currently written, requires DPH to collect and report data on residents and staff in nursing homes and other DPH long-term care facilities as well as correctional centers. But the bill does not mention DDS group homes.
As we’ve said before, we are concerned that even as Governor Baker cautiously reopens the Massachusetts economy based on encouraging data on the incidence of COVID-19 in the population of the state as a whole, the administration does not appear to be showing the same caution or concern for clients in the DDS system.
At the very least, DDS should adhere to written federal and state guidelines regarding testing of group home staff.
We are encouraging people to call the Public Health Committee, and urging them to support an amendment to Senator Eldridge’s bill (S.2657) that would make testing of DDS staff mandatory. The phone numbers are (617) 722-1532 for the office of the Senate chair of the committee, and (617) 722-2130 for the House chair.
